Living Clinical Guidelines for Stroke Management
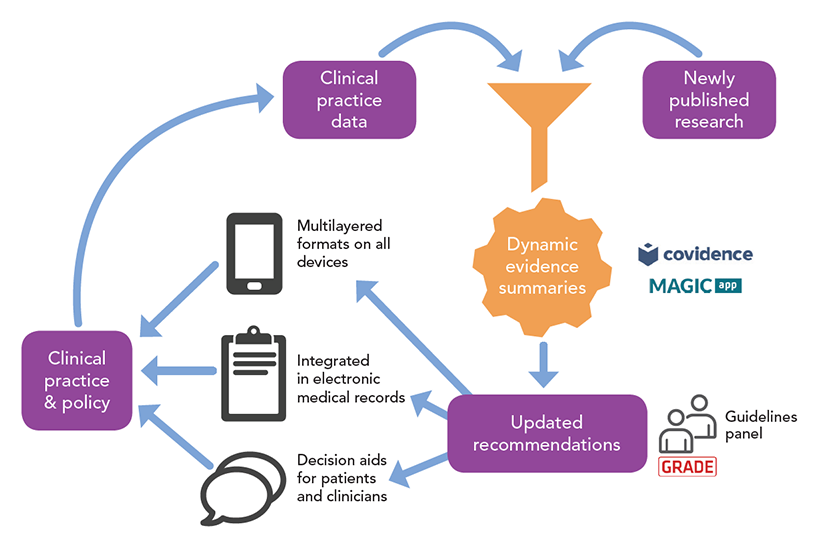 The Australian and New Zealand Clinical Guidelines for Stroke Management are living guidelines, updated as new evidence emerges. They supersede the 2017 Clinical Guidelines.
The Australian and New Zealand Clinical Guidelines for Stroke Management are living guidelines, updated as new evidence emerges. They supersede the 2017 Clinical Guidelines.
How to use the guidelines
- MAGICapp.org is the platform that hosts the guidelines. When you click a link you may be asked to accept terms and conditions, or to load the latest version. Please agree and continue to the guidelines.
- Save a PDF of the guidelines as they are today by clicking on the PDF link in the top right corner of MAGICapp.
- Version history of each recommendation can be seen by clicking the exclamation icon
 to its right, or you can see a description of changes in the version history of each chapter under the About link in the top right corner of MAGICapp.
to its right, or you can see a description of changes in the version history of each chapter under the About link in the top right corner of MAGICapp. - See a list of all updates, plus drafts for consultation.
If you have any questions, please contact guidelines@strokefoundation.org.au
Contents
The Clinical Guidelines cover the whole continuum of stroke care, across 8 chapters.
Chapter 1: Pre-hospital care
Chapter 2: Early assessment and diagnosis
- Clinical questions
- Early assessment and diagnosis - overview
- Transient ischaemic attack
- Assessment of suspected stroke
- Investigations
Chapter 3: Acute medical and surgical management
- Clinical questions
- Acute medical and surgical management - overview
- Stroke unit care
- Assessment for rehabilitation
- Palliation
- Reperfusion therapy
- Dysphagia
- Acute antithrombotic therapy
- Acute blood pressure lowering therapy
- Surgery for ischaemic stroke
- Intracerebral haemorrhage (ICH) management
- Oxygen therapy
- Brain cytoprotection
- Glycaemic therapy
- Pyrexia management
- Acute stroke telehealth services
- Head position
Chapter 4: Secondary prevention
- Clinical questions
- Secondary prevention - overview
- Adherence to pharmacotherapy
- Blood pressure lowering therapy
- Management of atrial fibrillation
- Antiplatelet therapy
- Cholesterol lowering therapy
- Carotid surgery
- Cervical artery dissection
- Cerebral venous thrombosis
- Diabetes management
- Patent foramen ovale management
- Hormone replacement therapy
- Oral contraception
- Lifestyle modifications
Chapter 5: Rehabilitation
- Clinical questions
- Rehabilitation - overview
- Commencement of rehabilitation
- Amount of rehabilitation
- Early supported discharge services
- Home-based rehabilitation
- Goal setting
- Sensorimotor impairments
- Activity limitations
- Participation restrictions
- Communication difficulties
- Cognition and perception difficulties
- Telehealth in rehabilitation
Chapter 6: Managing complications
- Clinical questions
- Managing complications - overview
- Nutrition and hydration
- Oral hygiene
- Spasticity
- Contracture
- Subluxation
- Pain
- Swelling of the extremities
- Fatigue
- Incontinence
- Mood disturbance
- Deep venous thrombosis or pulmonary embolism
- Falls
- Pressure injury
- Sleep disorders
Chapter 7: Discharge planning and transfer of care
- Clinical questions
- Discharge planning and transfer of care - overview
- Information and education
- Discharge care plans
- Patient and carer needs
- Home assessment
- Carer training
Chapter 8: Community participation and long-term care
- Clinical questions
- Community participation and long-term care - overview
- Self-management
- Driving
- Community mobility and outdoor travel
- Leisure
- Return to work
- Sexuality
- Support
Suggest a new topic or question
Have we missed anything important? To keep the living guidelines relevant, our project steering committee annually reviews the topics the guidelines cover and the questions about practice that they answer.
We welcome suggestions for new topics to consider during our annual review.
Please email your suggestions to guidelines@strokefoundation.org.au
Short summaries
Consumer resources
Discipline-specific summaries
- Dietetics
- Emergency department
- General practitioners
- Nursing
- Occupational therapy
- Pharmacy
- Physiotherapy
- Psychology
- Social work
- Speech pathology
Development process
Details of how we develop the guidelines, along with administrative and technical reports and other documents required for NHMRC approval, can be found under Guidelines development process.
This includes a current list of working group members and other people involved in developing the guidelines.
Implementation tools
In this video, the previous co-chair of the Guidelines Content Steering Group, Prof. Coralie English, explains the guidelines for stroke rehabilitation:
Suggested citation
Stroke Foundation. Australian and New Zealand Living Clinical Guidelines for Stroke Management. Available at https://informme.org.au/en/Guidelines/Clinical-Guidelines-for-Stroke-Management. Accessed [insert date, month and year and if applicable specific sections or chapters].
© No part of this publication can be reproduced by any process without permission from the Stroke Foundation. 2025.